The Short Answer: Magnesium deficiency can show up as muscle cramps, twitching, fatigue, poor sleep, or heart rhythm changes — and about 48–50% of U.S. adults fall short on magnesium intake. Blood tests often miss early deficiency, so symptoms and risk factors matter just as much.[1]
- Symptoms can be subtle — early signs often look like cramps, eyelid twitching, or low energy.
- Low intake is common — modern diets are one of the biggest drivers.
- Testing has limits — <1% of body magnesium circulates in blood.
- Fixing it is usually manageable — food first, supplements when needed, plus medication review.
Based on current research as of January 2026. This isn’t medical advice — it’s a starting point for a conversation with your healthcare provider. (How PharmaGuide reviews supplement safety)
What We’ll Cover
- Why magnesium matters so much in the body
- Early vs serious deficiency symptoms
- Who’s at higher risk — and why
- Why lab tests can be misleading
- How to fix deficiency safely
- Side effects, medication timing, and myths
Feeling muscle cramps, eyelid twitching, fatigue that won’t quit, or restless sleep? These can be early signs of magnesium deficiency — and millions of people have no idea they’re running low. Recognizing magnesium deficiency symptoms is important for early intervention and health management.
Magnesium deficiency is tricky because it doesn’t announce itself loudly at first. It creeps in quietly, often mistaken for stress, aging, poor sleep, or dehydration.
This guide will help you figure out whether magnesium could be part of what you’re feeling — and what to do about it safely, without guessing or megadosing.
How Magnesium Deficiency Actually Works (In Plain English)
Magnesium is a behind-the-scenes mineral. You don’t feel it when levels are good — but you often feel it when they drop.
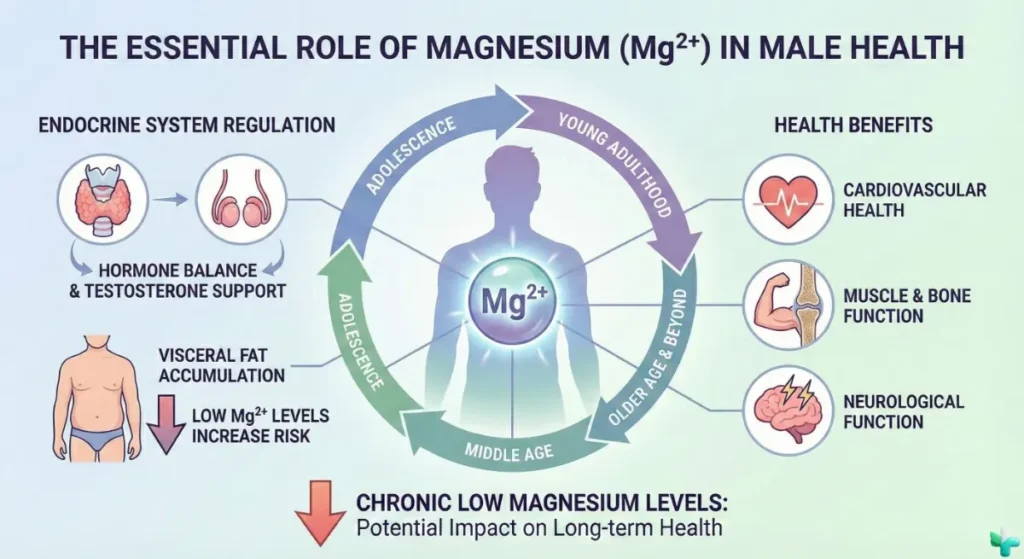
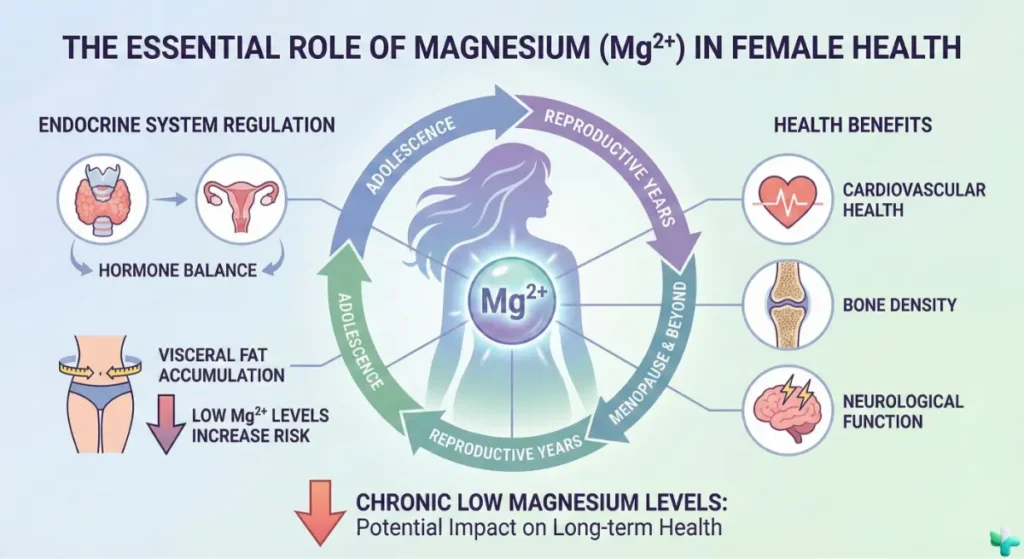
It acts as a helper for 300+ enzyme reactions involved in energy production (ATP), nerve signaling, muscle relaxation, blood sugar control, and heart rhythm stability.[1]
A simple way to think about it: magnesium helps muscles relax after they contract. When levels are low, muscles stay tense longer — which can show up as cramps, twitching, or that restless, wired feeling.
That last point matters. Most magnesium lives inside cells and bone. So a “normal” blood magnesium level doesn’t always mean your overall magnesium status is ideal — especially early on or if losses are ongoing.[4]
Magnesium also works closely with other electrolytes. If magnesium is low, potassium and calcium levels can become harder to stabilize — even if you’re supplementing them.[4]
What the Research Shows
The evidence is strong that magnesium is essential for muscle, nerve, and heart function. The evidence is moderate that supplementation may help cramps or sleep — mainly in people who are already low. If your baseline magnesium is fine, you may not feel much. If it’s low, the difference can be noticeable.
Magnesium Intake & Chronic Disease Risk
Moderate EvidenceKey Finding: Higher dietary magnesium intake is consistently associated with lower rates of type 2 diabetes, hypertension, and cardiovascular disease in large population studies.
How to Fix Magnesium Deficiency (Food, Supplements, and Smart Timing)
Correcting magnesium deficiency usually comes down to three steps: improve intake, supplement thoughtfully if needed, and identify what’s draining magnesium in the first place.
Step 1: Food First
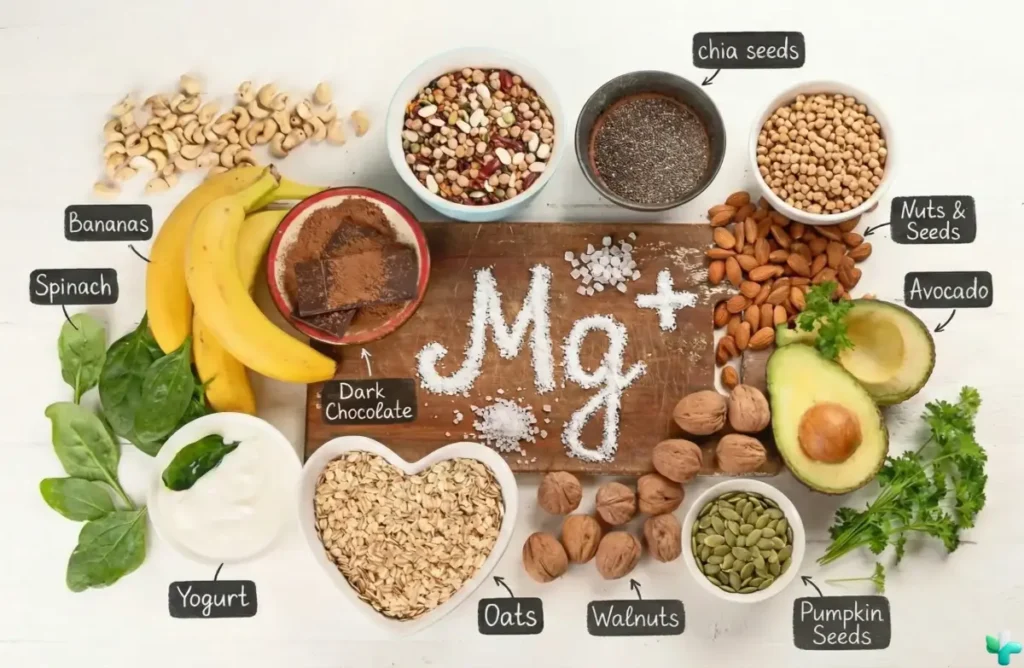
Magnesium-rich foods include leafy greens, beans, lentils, whole grains, nuts, seeds (especially pumpkin seeds), dairy, and some fish. Food-based magnesium is absorbed gradually and rarely causes side effects.[1]
Step 2: Choose a Supplement Form You’ll Tolerate
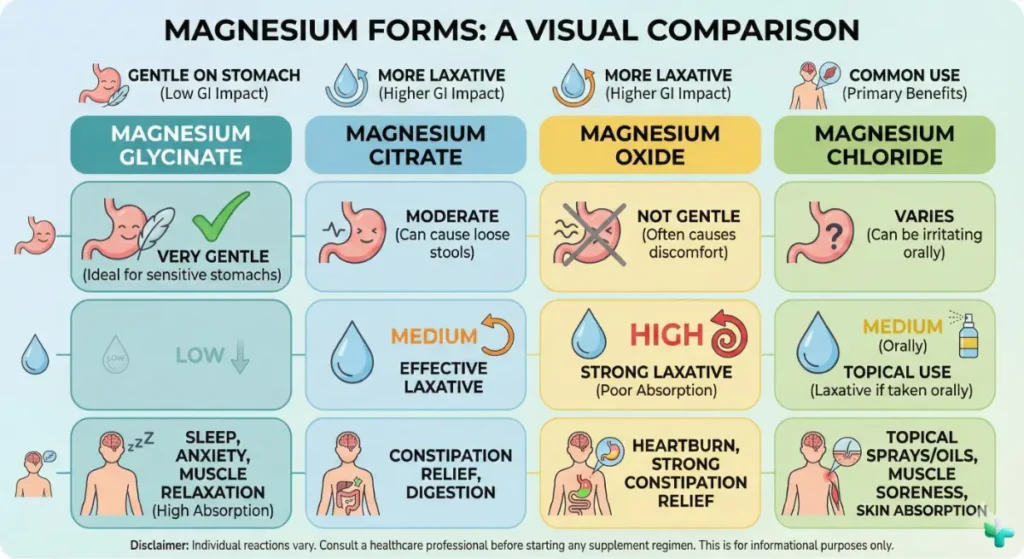
Why Magnesium Form Matters
Different magnesium forms behave very differently in the gut. Choosing the wrong one is the most common reason people quit magnesium.
- Magnesium glycinate: Gentle and well tolerated. Often preferred for sleep, muscle tension, and general deficiency.
- Magnesium citrate: Absorbs well but pulls water into the intestines. Helpful for constipation, but dose-sensitive.
- Magnesium oxide: Poor absorption and more GI side effects. Often acts more like a laxative.
| Form | Best For | Tradeoff |
|---|---|---|
| Magnesium glycinate | Sleep, tension, gentle repletion | Costs a bit more |
| Magnesium citrate | Constipation + deficiency | Loose stools at higher doses |
| Magnesium oxide | Budget or laxative use | Poor absorption, GI upset |
Step 3: Dosing & Timing
| Goal | Dose | Timing |
|---|---|---|
| General support | 100–200 mg/day | Evening or split dose |
| Muscle cramps | 200–300 mg/day | Split dosing preferred |
The NIH lists 350 mg/day as the tolerable upper limit for supplemental magnesium due to diarrhea risk. Food magnesium does not count toward this limit.[1]
Separate magnesium by at least 4 hours from antibiotics like ciprofloxacin or doxycycline to avoid reduced drug absorption.
Safety, Side Effects, and Who Should Be Careful
Magnesium is generally safe when used thoughtfully. Most issues come from taking too much too fast, choosing the wrong form, or using magnesium when the body can’t clear it properly.
Generally Well-Tolerated
- Magnesium from food rarely causes toxicity in healthy adults.
- Lower supplemental doses (100–200 mg/day) are usually easy to tolerate.
- Gentler forms like magnesium glycinate cause fewer GI issues for many people.
Potential Side Effects
- Diarrhea, cramping, or nausea — especially with higher doses or forms like oxide and citrate.
- Lightheadedness or low blood pressure if magnesium levels rise too high.
- Masking the real problem if magnesium loss continues unchecked (for example, chronic diarrhea or medication effects).
Who Should Talk to a Doctor or Pharmacist First
Magnesium deserves extra caution if any of the following apply to you:
- Kidney disease or reduced kidney function — impaired clearance raises the risk of magnesium accumulation.[4]
- Chronic diarrhea or malabsorption — ongoing losses may require lab monitoring and tailored dosing.[2]
- Alcohol use disorder — a common but often overlooked cause of low magnesium.[4]
Medication timing also matters. Speak with your pharmacist if you take:
- Diuretics (such as furosemide) — increase urinary magnesium loss.
- Proton pump inhibitors (PPIs) (like omeprazole or pantoprazole) — long-term use has been linked to low magnesium in some patients.
- Antibiotics — separate magnesium from ciprofloxacin, levofloxacin, and doxycycline by at least 4 hours.
- Bisphosphonates (such as alendronate) — minerals can interfere with absorption if taken together.
When to Stop and Get Medical Help
Seek urgent care for chest pain, fainting, new or worsening heart palpitations, seizures, severe weakness, or confusion. These may signal a serious electrolyte imbalance or heart rhythm issue and should not be managed with supplements alone.
Myths and Misconceptions
Myth #1: “If I’m tired or anxious, it must be magnesium deficiency.”
The reality: fatigue and anxiety are common and non-specific. Magnesium can play a role, but so can sleep debt, iron deficiency, thyroid disease, depression, dehydration, or medication side effects.
Myth #2: “More magnesium means better sleep.”
The reality: magnesium may help sleep quality in people who are low, but it’s not a sedative. Higher doses often worsen sleep by causing GI distress.
Myth #3: “A normal blood magnesium test means I’m fine.”
The reality: serum magnesium reflects less than 1% of total body stores. Symptoms and risk factors still matter, even when labs appear normal.

The Bottom Line
Magnesium deficiency is common, underdiagnosed, and often misunderstood. Early signs can feel mild — cramps, twitching, fatigue, poor sleep — but prolonged deficiency can affect heart rhythm, nerve function, and overall metabolic health.
If your diet is low in whole foods, or you use medications like PPIs or diuretics, magnesium is worth a closer look. Start with food, supplement conservatively if needed, and pay attention to medication timing and tolerance.
One simple next step: track your magnesium intake for a few days, add one magnesium-rich food daily, and if you supplement, start low (100–200 mg/day). If symptoms are severe or cardiac-related, skip self-experimentation and contact your clinician.
Key Takeaways
- Magnesium supports muscle relaxation, nerve signaling, energy production, and heart rhythm.
- About half of U.S. adults fall short on magnesium intake.
- Blood tests can miss early or functional deficiency.
- Food-first plus smart supplementation is usually effective and safe.
Want to keep learning? Explore more guides in our Health Education hub.
Common Questions
What are the most common magnesium deficiency symptoms?
Muscle cramps, twitching, fatigue, weakness, and poor sleep are common early signs. More severe deficiency can affect heart rhythm and the nervous system.
How can I tell if magnesium deficiency is causing my symptoms?
A blood test can help, but it’s not definitive. Clinicians also consider diet, medications, GI symptoms, alcohol use, and related electrolyte levels.
What’s the safest magnesium supplement to start with?
Magnesium glycinate is often a good first choice due to better tolerance. Citrate may help constipation but requires careful dosing.
How much magnesium should I take daily?
Most adults start with 100–200 mg/day of elemental magnesium. The tolerable upper limit for supplements is 350 mg/day due to diarrhea risk.
Can magnesium interact with medications?
Yes. Magnesium can interfere with absorption of certain antibiotics and bone medications. Spacing doses by several hours is often required.
When is magnesium unsafe?
Magnesium can be unsafe in kidney disease or when taken in very high doses. Symptoms like confusion, severe weakness, or heart rhythm changes need urgent evaluation.
Take the Guesswork Out of Supplements
Understanding magnesium deficiency is just the start. PharmaGuide’s AI Pharmacist analyzes your complete health profile to give you personalized, evidence-based recommendations.
Join the Waitlist →